



Business Inquiry
Global:
Email:marketing@medicilon.com
+1(781)535-1428(U.S.)
0044 7790 816 954 (Europe)
China:
Email: marketing@medicilon.com.cn
Tel: +86 (21) 5859-1500



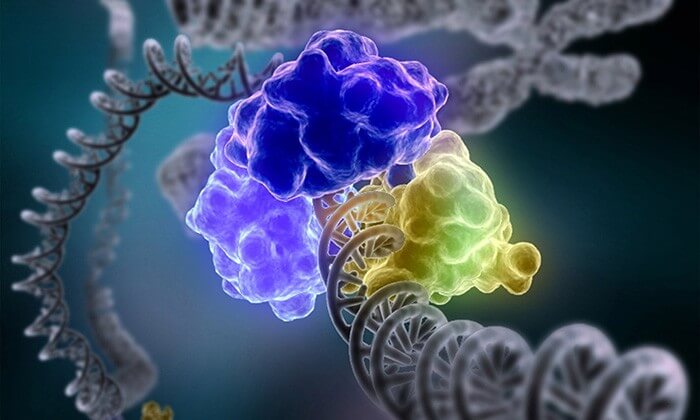
The busy world inside a cell is directed by its DNA blueprint. When the blueprints are altered, cells can sicken, die or become cancerous. To keep DNA in working order, cells have ways to detect and mend damaged DNA.
Chemotherapy could be more effective if combined with the inhibition of a newly discovered form of DNA repair, a mechanism that cells activate to fix precisely the sort of damage that many chemotherapy drugs cause – or are supposed to cause. The relevant chemotherapy drugs are alkylating agents, which try to kill cancer cells by adding alkyl groups to DNA. These debilitating accretions, however, can be removed by an alkylation repair complex.
This repair complex is recruited to damage sites via a signaling pathway recently described by scientists at the Washington University School of Medicine in St. Louis. The scientists reported their findings in the journal Nature in an article entitled “A Ubiquitin-Dependent Signalling Axis Specific for ALKBH-Mediated DNA Dealkylation Repair.”
The article notes that although biochemical mechanisms for repairing several forms of genomic insults are well understood, essential gaps in our knowledge remain. Although we are familiar with the upstream signaling pathways that account for certain kinds of DNA damage – double-stranded breaks and interstrand cross-links – we are less sure about other types of DNA damage, including the damage wrought by alkylating agents.
Alkylation can happen naturally, which is why cells have this repair system in the first place. Also, certain chemotherapy drugs force it to happen. Busulfan is used to treat leukemia, and temozolomide, prescribed for brain tumors, alkylates many spots along DNA. It is difficult for the genetic blueprint to be copied accurately where DNA has been alkylated, so alkylation damage kills the cells.
By inflicting alkylation damage, chemo attempts to overwhelm the cells’ ability to heal themselves. Yet chemo may fail to inflict sufficient lasting damage unless the cells’ DNA dealkylation repair mechanism is somehow thwarted. As it happens, some tumors are abnormally dependent on the proteins involved in this DNA repair, so knocking out those proteins kills the tumor cells.
Medicilon boasts nearly 300 tumor evaluation models. At the same time, we are empowering innovative therapies to comprehensively evaluate and study immuno-oncology. We have completed model establishment and efficacy evaluation of immuno-therapies such as CAR-T, TCR-T, CAR-NK, oncolytic virus, antibody (monoclonal antibody, double antibody, polyclonal antibody, etc.), siRNA, AAV.
Tumor Animal Model Medicilon Has Established:“We found that human cells can sense alkylation damage and mobilize a repair complex specifically suited to repair this kind of injury,” said the Nature article’s senior author, Nima Mosammaparast, M.D., Ph.D., an assistant professor of pathology and immunology. “Knocking out this complex may be a way to increase the potency of certain chemotherapy drugs or to specifically target tumor cells that have become dependent on the repair complex.”
Studying cells treated with alkylating chemotherapy drugs or drugs that lead to other kinds of DNA damage, the researchers determined how cells try to mend DNA damage caused specifically by alkylating agents. They identified a group of proteins that clustered near the spots on the DNA that had been alkylated.
“We find that the alkylation repair complex ASCC (activating signal integrator complex) relocalizes to distinct nuclear foci specifically upon exposure of cells to alkylating agents,” wrote the article’s authors. “These foci associate with alkylated nucleotides and coincide spatially with elongating RNA polymerase II and splicing components.”
Cells that lacked a vital member of this protein complex were more likely to die if treated with alkylating drugs than cells with the protein, indicating the importance of the protein complex in repairing DNA. Lacking the essential protein made no difference when the DNA was damaged in other ways.
“Proper recruitment of the repair complex requires recognition of K63-linked polyubiquitin by the CUE (coupling of ubiquitin conjugation to ER degradation) domain of the subunit ASCC2,” continued. “Loss of this subunit impedes alkylation adduct repair kinetics and increases sensitivity to alkylating agents, but not other forms of DNA damage.”
These findings suggest that sensing alkylation damage is a primary defense against chemotherapy drugs such as busulfan and other alkylating agents. Interfering with this repair complex could amplify the killing power of such drugs and potentially even avert or undermine drug resistance. After a successful course of chemotherapy, tumors sometimes recur more challenging than before, having become resistant to the drugs from the first round of treatment.
“There’s some evidence now that overexpressing components of this signaling pathway may be how some tumors become resistant to chemotherapy,” Mosammaparast said. “Blocking this pathway could be a way to make resistant tumors sensitive again.”
Recurrent tumors are not the only ones that may have high levels of DNA repair proteins. Some tumors that have never encountered alkylating chemotherapy drugs have high levels of critical alkylation-repair proteins. And when they do, it portends poorly for the patients.
“In some kinds of pancreatic, prostate, and lung cancer, overexpressing components of this pathway indicates a significantly worse prognosis,” Mosammaparast noted.
There is a possible silver lining, though. Tumors with high levels of essential alkylation repair proteins often depend on them, meaning that if those proteins were somehow inhibited, the cells would die. Normal cells are not dependent on this alkylation repair pathway to the same degree. Other repair systems can handle the level of alkylating DNA damage typically encountered by a healthy cell.
“That could be an opening for a chemotherapy drug,” Mosammaparast said. “We may be able to design a toxic drug to tumors but not to normal cells by targeting this alkylation repair pathway.”
The drug olaparib, approved in 2014 to treat hereditary ovarian cancer, exploits a similar vulnerability. It targets tumors that are unusually dependent on a repair pathway that stitches DNA back together after cutting it into pieces. Olaparib blocks that pathway, and without it, the cancerous cells die.
 Relevant
news
Relevant
news