



Business Inquiry
Global:
Email:marketing@medicilon.com
+1(781)535-1428(U.S.)
0044 7790 816 954 (Europe)
China:
Email: marketing@medicilon.com.cn
Tel: +86 (21) 5859-1500



University of Wyoming researchers say they have found that mice engineered to have Huntington’s disease (HD) have an over-accumulation of iron in their mitochondria. Their work identifying a pathway for the neurodegenerative disease also has relevance to understanding related disorders such as Parkinson’s, Alzheimer’s, and Lou Gehrig’s diseases, says Jonathan Fox, Ph.D., a professor in the University of Wyoming’s Department of Veterinary Sciences.
The team’s study (“Brain Mitochondrial Iron Accumulates in Huntington’s Disease, Mediates Mitochondrial Dysfunction, and Can Be Removed Pharmacologically”) is published online in Free Radical Biology and Medicine.
“Mitochondrial bioenergetic dysfunction is involved in neurodegeneration in Huntington’s disease (HD). Iron is critical for normal mitochondrial bioenergetics but can also contribute to pathogenic oxidation. The accumulation of iron in the brain occurs in mouse models and in human HD. Yet the role of mitochondria-related iron dysregulation as a contributor to bioenergetic pathophysiology in HD is unclear. We demonstrate here that human HD and mouse model HD (12-week R6/2 and 12-month YAC128) brains accumulated mitochondrial iron and showed increased expression of iron uptake protein mitoferrin 2 and decreased iron-sulfur cluster synthesis protein frataxin. Mitochondria-enriched fractions from mouse HD brains had deficits in membrane potential and oxygen uptake and increased lipid peroxidation. In addition, the membrane-permeable iron-selective chelator deferiprone (1 μM) rescued these effects ex-vivo, whereas hydrophilic iron and copper chelators did not. A 10-day oral deferiprone treatment in 9-week R6/2 HD mice indicated that deferiprone removed mitochondrial iron, restored mitochondrial potentials, decreased lipid peroxidation, and improved motor endurance,” write the investigators.
“Neonatal iron supplementation potentiates neurodegeneration in mouse models of HD by unknown mechanisms. We found that neonatal iron supplementation increased brain mitochondrial iron accumulation and potentiated markers of mitochondrial dysfunction in HD mice. Therefore, bi-directional manipulation of mitochondrial iron can potentiate and protect against markers of mouse HD. Our findings thus demonstrate the significance of iron as a mediator of mitochondrial dysfunction and injury in mouse models of human HD and suggest that targeting the iron-mitochondrial pathway may be protective.”
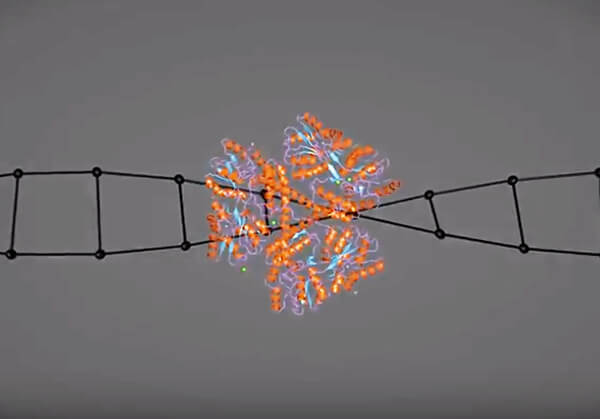
Mitochondria are a main site of oxygen use in cells. The scientists measured oxygen consumption in mouse HD mitochondria and found oxygen deficits in HD mitochondria with unusual amounts of iron. The research suggests iron accumulation in mitochondria interferes with respiration and oxygen uptake, and that this may contribute to neuronal malfunction and death.
Excess iron in cells can be detrimental, but adequate iron supplies also are essential to many cell functions.
“A wide variety of different proteins require iron,” says Dr. Fox, who also teaches in the university’s Wyoming, Washington, Alaska, Montana, and Idaho (WWAMI) medical program. “Probably the best known is hemoglobin. The protein requires iron to transport oxygen properly. Iron metabolism is central for normal cell function.”
The flip side is that too much can be toxic. Cells are challenged to provide iron for functions that require it but also prevent toxic accumulations.
“In HD, we think that normal iron metabolism is disrupted, and these adverse effects of iron are allowed to continue,” notes Dr. Fox, adding that this pathway is not the only factor that drives HD.
“There are many other pathways that have been shown to be important,” he continues. “We’re saying this is an important part of the picture.”
Dr. Fox points out that the research helps lay the foundation for developing drug therapies.
“Mouse HD models are great for studying the human disease but are not perfect,” he says. “Whenever possible, we try to verify that the findings in animal models are actually present in the human condition. We were fortunate enough to obtain human brain tissue and show similar changes to the HD mice in the current study.”
The scientists also are interested in environmental factors that can affect HD. Their latest paper adds to previous work showing high iron intake by HD mice early in life promotes the disease in adulthood.
Still, Dr. Fox says the researchers in his lab are interested in pursuing two areas. They want to further understand the mechanisms by which iron causes mitochondrial dysfunction in HD. The other, broader aspect is that HD is part of a group of related diseases, and “while they don’t have identical mechanisms, they do have some important features in common. So, we are interested in determining if mitochondrial iron accumulation occurs in models of Parkinson’s, Alzheimer’s, and brain aging. We are interested in expanding beyond HD mouse models.”
 Relevant
news
Relevant
news