



A neurological disorder is any disorder of the nervous system. Structural, biochemical or electrical abnormalities in the brain, spinal cord or other nerves can result in a range of symptoms.
Researchers at Case Western Reserve University School of Medicine have successfully grown stem cells from children with a devastating neurological disease to help explain how different genetic backgrounds can cause similar symptoms.
The work sheds light on how certain brain disorders develop, and provides a framework for developing and testing new therapeutics. Medications that appear promising when exposed to the new cells could be precisely tailored to individual patients based on their genetic background.
In the new study (“Modeling the Mutational and Phenotypic Landscapes of Pelizaeus-Merzbacher Disease with Human iPSC-Derived Oligodendrocytes”), published in The American Journal of Human Genetics, investigators used stem cells in their laboratory to simultaneously model different genetic scenarios that underlie neurologic disease. They identified individual and shared defects in the cells that could inform treatment efforts.
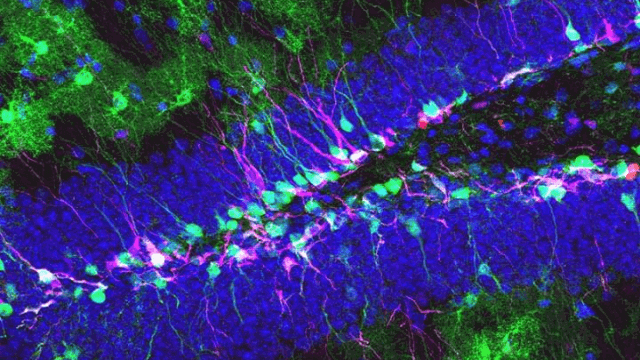
The team developed induced pluripotent stem cells (iPSCs) from 12 children with various forms of Pelizaeus-Merzbacher disease (PMD). The rare but often fatal genetic disease can be caused by one of hundreds of mutations in a gene critical to the proper production of nerve cell insulation, or myelin. Some children with PMD have missing, partial, duplicate, or even triplicate copies of this gene, while others have only a small mutation. With so many potential causes, researchers have been in desperate need of a way to accurately and efficiently model genetic diseases like PMD in human cells.
By recapitulating multiple stages of the disease in their laboratory, the scientists established a broad platform for testing new therapeutics at the molecular and cellular level. They were also able to link defects in brain cell function to patient genetics.
“Stem cell technology allowed us to grow the cells that make myelin in the laboratory directly from individual PMD patients. By studying a wide spectrum of patients, we found that there are distinct patient subgroups. This suggests that individual PMD patients may require different clinical treatment approaches,” said Paul Tesar, Ph.D., study lead, Drs. Donald and Ruth Weber Goodman Professor of Innovative Therapeutics, and associate professor of genetics and genome sciences at Case Western Reserve University School of Medicine.
The researchers watched in real-time as the patients’ stem cells matured in the laboratory. “We leveraged the ability to access patient-specific brain cells to understand why these cells are dysfunctional. We found that a subset of patients exhibited an overt dysfunction in certain cellular stress pathways,” said Zachary Nevin, first author of the study and M.D./Ph.D. student at Case Western Reserve University School of Medicine. “We used the cells to create a screening platform that can test medications for the ability to restore cell function and myelin. Encouragingly, we identified molecules that could reverse some of the deficits.”
The finding provides proof-of-concept that medications that mend a patient’s cells in the laboratory could be advanced to clinical testing in the future.
The stem cell platform could also help other researchers study and classify genetic diseases with varied causes, particularly other neurologic disorders. Said Dr. Tesar, “Neurological conditions present a unique challenge, since the disease-causing cells are locked away in patients’ brains and inaccessible to study. With these new patient-derived stem cells, we can now model disease symptoms in the laboratory and begin to understand ways to reverse them.”
 Relevant
news
Relevant
news