



Business Inquiry
Global:
Email:marketing@medicilon.com
+1(781)535-1428(U.S.)
0044 7790 816 954 (Europe)
China:
Email: marketing@medicilon.com.cn
Tel: +86 (21) 5859-1500



Using state-of-the-art genomics tools, researchers have pinpointed genes that contribute to antibiotic resistance in two global superbugs. They show how such a discovery could lead to “helper drugs” with the potential to restore the susceptibility of resistant bacteria to antibiotics.
In the fight against antibiotic drug resistance, researchers have often devised clever methods to circumvent the adaptive properties of superbugs—bacteria that have developed resistance to the vast majority of current drug therapies.
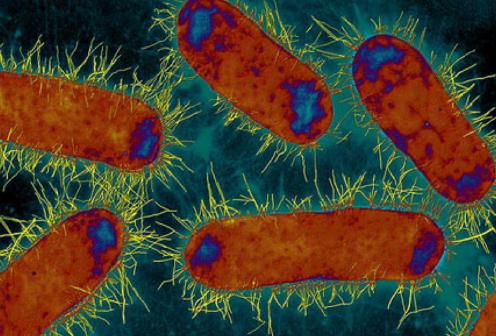
Now, a team of researchers at the University of Copenhagen and Ross University School of Veterinary Medicine have discovered a new way to restore antibiotic susceptibility in multidrug-resistant (MDR) Klebsiella pneumoniae—a main cause of fatal lung and bloodstream infections worldwide—and Escherichia coli strains. Results from the new study were published recently in two peer-reviewed journals. The first is in Scientific Reports in an article entitled “The Secondary Resistome of Multidrug-Resistant Klebsiella pneumoniae” and the second in Antimicrobial Agents and Chemotherapy in an article entitled “Cephem Potentiation by Inactivation of Non-Essential Genes Involved in Cell Wall Biogenesis of β-Lactamase-Producing Escherichia coli.”
“Our discovery shows that resistant superbugs are not invincible,” explained senior investigator on both studies Luca Guardabassi, D.V.M., Ph.D., professor in the department of veterinary clinical and animal sciences at the University of Copenhagen and director of One Health Center for Zoonoses and Tropical Veterinary Medicine at Ross University. “They have an Achilles heel, and now we know how to defeat them.”
Using high-powered genomics, the research team measured the contribution of every bacterial gene toward antibiotic resistance, leading to the identification of several genes that are vital for the survival of MDR K. pneumoniae in the presence of colistin, the last-resort antibiotic for treating infections caused by these bacteria. As a proof of principle, it was shown that inactivation of one of these genes, dedA, made colistin-resistant MDR K. pneumoniae completely sensitive to this antibiotic. Moreover, the investigators also discovered similar genes that upon inactivation restored the susceptibility to β-lactam antibiotics in MDR E. coli.
Dr. Guardabassi and his colleagues are hopeful that these findings will open new perspectives on the possibility to defeat resistant superbugs by combining antibiotics with “helper” drugs that reverse antibiotic resistance. To date, the β-lactamase inhibitors are the only type of antibiotic helper drugs used in clinical practice. These drugs reverse antibiotic resistance by inhibiting the bacterial enzyme responsible for degradation of the β-lactam antibiotics. Different from β-lactamase inhibitors, the targets identified in the two studies are not directly implicated in the mechanism of antibiotic resistance.
“In contrast to β-lactamase inhibitors, the antibiotic helper drugs conceptualized by our research would also improve the efficacy of the ‘helped’ antibiotic against susceptible strains,” Dr. Guardabassi noted. “This is a desirable feature for a helper drug as it would reduce the risk of treatment failure due to factors other than antibiotic resistance (e.g., biofilms, immunosuppression, etc.), allow dose reduction for toxic antibiotics such as colistin, and possibly even prevent selection of resistant mutants.”
The latter hypothesis is presently under study using colistin in combination with an antifungal drug that is known to interfere with one of the targets identified by this research in MDR K. pneumoniae.
“It is extremely important to contain the threat posed by MDR bacteria,” remarked Anders Miki Bojesen, Ph.D., professor in the department of veterinary clinical and animal sciences at the University of Copenhagen, who was not directly involved in the current studies. “These new results create optimism for the future treatment of infectious diseases. Ahead of us now is the major task of exploring the potential of new drug targets, so that hopefully we can prevent the number of people with untreatable infections from escalating further.”
 Relevant
news
Relevant
news