


As of Beijing time The data is from a third-party organization and is only for reference.
For actual information, please refer to:www.eastmoney.com
Address: 20 Maguire Road, Suite 103, Lexington, MA 02421(America)
Tel: +1(626)986-9880
Address: Allia Future Business Centre Kings Hedges Road Cambridge CB4 2HY, UK
Tel: 0044 7790 816 954
Email: marketing@medicilon.com
Address: No.585 Chuanda Road, Pudong New Area, Shanghai (Headquarters)
Postcode: 201299
Tel: +86 (21) 5859-1500 (main line)
Fax: +86 (21) 5859-6369
© 2023 Shanghai Medicilon Inc. All rights reserved Shanghai ICP No.10216606-3
Shanghai Public Network Security File No. 31011502018888 | Website Map


Business Inquiry
Global:
Email:marketing@medicilon.com
+1(626)986-9880(U.S.)
0044 7790 816 954 (Europe)
China:
Email: marketing@medicilon.com.cn
Tel: +86 (21) 5859-1500



Patients successfully treated for breast, colon and other cancers can go on to develop an often-fatal form of leukemia, sometimes years after completion of treatment, due to a genetic mutation leading to secondary malignancies known as therapy-related myeloid neoplasms (t-MNs). While risk factors for the development of t-MNs are currently not well understood, a new study conducted by researchers at The University of Texas MD Anderson Cancer Center has revealed that preleukemic mutations, called clonal hematopoiesis, may predict whether patients develop the aggressive condition.
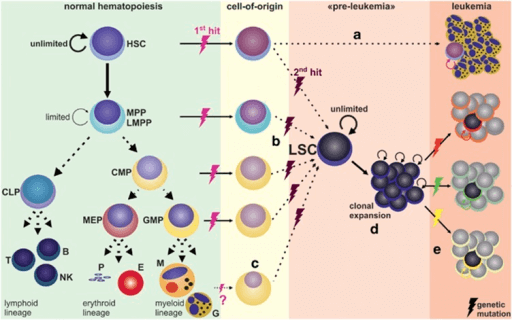
The researchers found that clonal hematopoiesis appears to function as a biomarker for patients who develop t-MNs, which is recognized for its extremely poor prognosis. The findings from this study were published recently in The Lancet Oncology in an article entitled “Preleukaemic Clonal Haemopoiesis and Risk of Therapy-Related Myeloid Neoplasms: A Case-Control Study.”
“Therapy-related myeloid neoplasms occur in about 5% of cancer patients who are treated with chemotherapy and/or radiation therapy,” explained senior study investigator Andy Futreal, Ph.D., chair ad interim of genomic medicine at The University of Texas MD Anderson Cancer Center. “In most cases, it is fatal, and currently there is no way to predict who is at risk or prevent it.”
The ability to detect t-MNs earlier is critical, given that the disease usually occurs 3 to 8 years following the completion of chemotherapy and/or radiation therapy.
“t-MNs are a problem that needs urgent attention,” noted lead study investigator Koichi Takashi, M.D., assistant professor of leukemia and genomic medicine at The University of Texas MD Anderson Cancer Center. “Since many cancer patients are now living longer, t-MNs are an increasing concern for many cancer survivors.”
The investigators studied 14 patients with t-MNs and found traces of preleukemic mutations or clonal hematopoiesis in 10. To determine if preleukemic mutations could reliably predict whether the patients would develop leukemia, the researchers compared the prevalence of preleukemic mutations in the 14 patients with 54 patients who did not develop t-MNs after therapy.
“We found that prevalence of preleukemic mutations was significantly higher in patients who developed t-MNs (71%) versus those who did not (26%),” Dr. Futreal remarked. “We also validated these findings in a separate cohort of patients. Based on these findings, we believe preleukemic mutations may function as a new biomarker that would predict t-MNs development.”
In the sample of 14 patients with t-MNs, the team looked at samples of bone marrow at the time of t-MNs development and blood samples obtained at the time of their primary cancer diagnosis. Through rigorous statistical analysis models on the external cohort, the researchers found that the presence of clonal hematopoiesis significantly increased the risk of therapy-related myeloid neoplasm development.
“We found genetic mutations that are present in t-MNs leukemia samples actually could be found in blood samples obtained at the time of their original cancer diagnosis,” Dr. Takahashi concluded. “Based on this finding, we believe the data suggest potential approaches of screening for clonal hematopoiesis in cancer patients that may identify patients at risk of developing t-MNs, although further studies are needed.”
 Relevant
news
Relevant
news